Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is amerigroup prior authorization form?
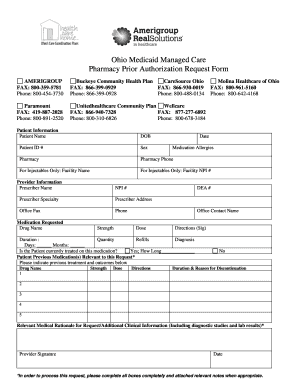
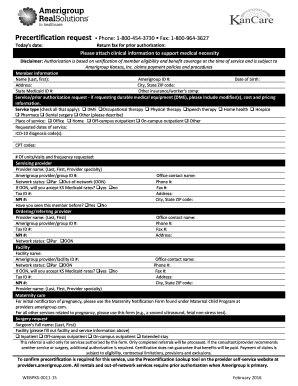
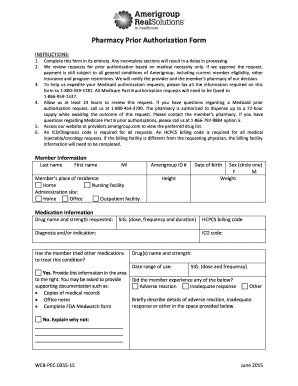
Amerigroup prior authorization form is a document that is required by the Amerigroup health insurance company to be completed by a healthcare provider before certain medical services or treatments can be approved and covered by the insurance. The form typically includes information about the patient, the healthcare provider, the specific services or treatments being requested, and supporting documentation such as medical records or test results. The purpose of the prior authorization process is to ensure that the requested services are medically necessary and meet the coverage criteria set by the insurance company.
Who is required to file amerigroup prior authorization form?
The Amerigroup prior authorization form is typically required to be filed by healthcare providers. This includes physicians, hospitals, clinics, and other healthcare facilities or professionals who are seeking authorization for certain medical procedures, treatments, medications, or services for their Amerigroup-insured patients.
How to fill out amerigroup prior authorization form?
To fill out an Amerigroup prior authorization form, follow these steps:
1. Obtain the form: You can obtain the prior authorization form from Amerigroup's website or by contacting their customer service line.
2. Section 1: Fill out the member information section, including the member's name, date of birth, member ID number, and contact information.
3. Section 2: Provide the provider information, including the name, address, phone number, and national provider identifier (NPI) number.
4. Section 3: Indicate the service being requested for prior authorization. Provide a detailed description of the service or procedure, including any diagnosis codes and CPT or HCPCS codes.
5. Section 4: Provide any supporting documentation that may be required, such as medical records, clinic notes, imaging reports, or lab results. Make sure to attach all relevant documentation to the form.
6. Section 5: Indicate the requested start and end date for the service or procedure, as well as any additional comments or notes.
7. Section 6: Have the provider or authorized staff member sign and date the form. Some forms may require additional signatures, such as the member's or guardian's signature.
8. Section 7: If necessary, provide information on additional providers involved in the member's care.
9. Submit the form: Send the completed prior authorization form, along with any supporting documentation, to Amerigroup through the specified channels. This may involve mailing, faxing, or submitting online through their secure portal.
It's essential to carefully review the form and ensure all information is accurate and complete before submission. Contact Amerigroup's customer service if you have any questions or need assistance filling out the form.
What is the purpose of amerigroup prior authorization form?
The purpose of the Amerigroup prior authorization form is to obtain approval from Amerigroup, a health insurance provider, before receiving certain medical services, procedures, medications, or equipment. The form serves as a request for prior authorization to ensure that the proposed treatment is medically necessary and covered under the individual's insurance plan. It helps the insurance provider assess the appropriateness and cost-effectiveness of the requested services, ensuring that they meet the company's guidelines and criteria for coverage. Obtaining prior authorization helps avoid surprises, ensures proper utilization, and allows the insurance company to manage costs and medical necessity effectively.
What information must be reported on amerigroup prior authorization form?
The specific information required on an Amerigroup prior authorization form may vary depending on the specific services or medications being requested. However, generally, the following information may need to be reported:
1. Member Information: This includes the name, address, date of birth, member ID number, and contact information of the patient who is requesting the prior authorization.
2. Prescriber Information: This includes the name, address, phone number, and National Provider Identifier (NPI) of the prescribing healthcare provider.
3. Diagnosis: The specific medical condition or reason for the requested service or medication must be provided along with the corresponding ICD-10 (International Classification of Diseases, 10th edition) diagnosis code.
4. Medication or Service Details: The name, strength, dosage, and quantity of the medication or service being requested should be included. If it is a medication, the pharmacy name and address may also need to be provided.
5. Supporting Documentation: Any relevant medical records, lab results, progress notes, or other documentation that supports the need for the requested service or medication should be attached to the prior authorization form.
6. Clinical Justification: A detailed explanation of why the requested service or medication is medically necessary and how it will benefit the patient's health should be included.
7. Insurance Information: The insurance policy information, including the group and policy numbers, must be provided to ensure accurate verification and processing.
It is important to consult the specific requirements and guidelines provided by Amerigroup for accurate and complete reporting on their prior authorization forms.
What is the penalty for the late filing of amerigroup prior authorization form?
The penalty for late filing of an Amerigroup prior authorization form can vary depending on the specific circumstances and policies of Amerigroup. It is best to refer to Amerigroup's guidelines or contact them directly to determine the exact penalty for late filing.
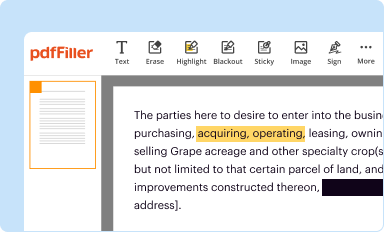
How can I edit amerigroup authorization form from Google Drive?
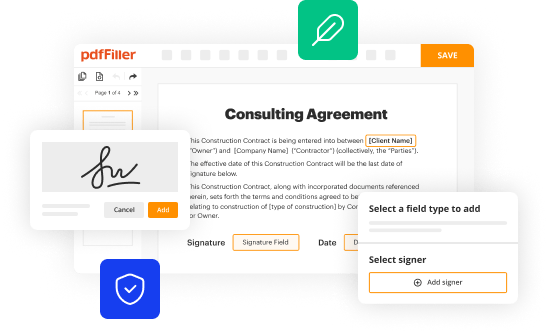
By integrating pdfFiller with Google Docs, you can streamline your document workflows and produce fillable forms that can be stored directly in Google Drive. Using the connection, you will be able to create, change, and eSign documents, including amerigroup prior authorization form, all without having to leave Google Drive. Add pdfFiller's features to Google Drive and you'll be able to handle your documents more effectively from any device with an internet connection.
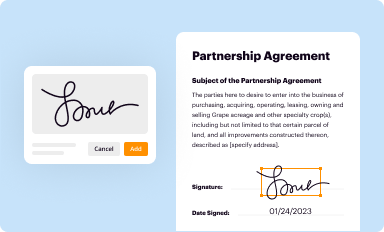
How do I complete amerigroup medicare prior authorization form on an iOS device?
pdfFiller has an iOS app that lets you fill out documents on your phone. A subscription to the service means you can make an account or log in to one you already have. As soon as the registration process is done, upload your amerigroup precert form. You can now use pdfFiller's more advanced features, like adding fillable fields and eSigning documents, as well as accessing them from any device, no matter where you are in the world.
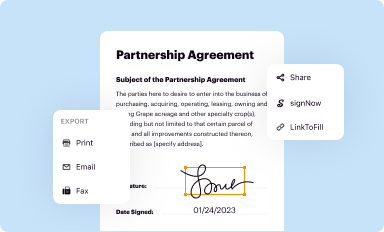
Can I edit amerigroup prior authorization form pdf on an Android device?
You can edit, sign, and distribute amerigroup authorization form 2020 on your mobile device from anywhere using the pdfFiller mobile app for Android; all you need is an internet connection. Download the app and begin streamlining your document workflow from anywhere.